The Centers for Medicare & Medicaid Services (CMS) has launched a new initiative: the Wasteful and Inappropriate Service Reduction (WISeR) Model, to reduce unnecessary spending in Original Medicare. Instead of altering existing coverage or payment rules, the WISeR Model targets low-value services by enhancing the prior authorization (PA) process.
Why Does This Matter?
- According to CMS, up to 25% of U.S. healthcare spending towards services that provide little to no value.
- In 2022 alone, the Medicare Payment Advisory Commission estimated that $5.8 billion was spent on minimally beneficial services.
- The WISeR Model aims to prevent wasteful care before it happens – not by limiting coverage, but by applying smarter review tools and processes.
What is the WISeR Model?
The WISeR Model is a new CMS initiative that leverages artificial intelligence (AI) and machine learning to flag low-value or potentially fraudulent services in Medicare. While technology plays a critical role in identifying questionable claims, licensed clinicians will make all final authorization decisions.
Importantly, this model:
- Does not change existing Medicare coverage or payment structures.
- Excludes emergency and high-risk services where delays could jeopardize patient safety.
Goals of the WISeR Model
The WISeR Model is built on four key goals:
- Direct Medicare spending toward services that truly improve patient outcomes.
- Adopt advanced, technology-driven review systems, modeled after commercial payer practices.
- Increase transparency around how Medicare coverage decisions are made.
- Reduce unnecessary or low-value care that drives up healthcare costs.
How the WISeR Model Works
Participation
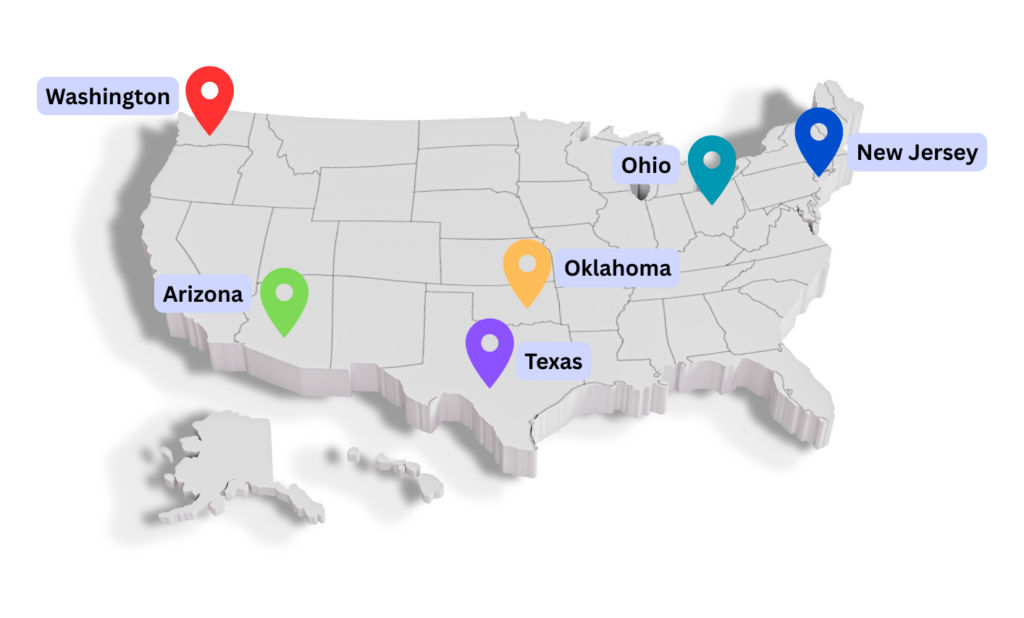
The WISeR Model will pilot in the following six states:
- Arizona
- New Jersey
- Ohio
- Oklahoma
- Texas
- Washington
Providers and suppliers in these states can choose to:
- Submit a prior authorization (PA) request before delivering targeted services; or
- Allow post-service, pre-payment review of claims before reimbursement.
Providers who demonstrate consistent compliance may earn a “gold card” exemption, removing the need for future reviews and reducing administrative overhead.
Technology-Powered Review
CMS is partnering with private technology firms that utilize AI and advanced analytics to evaluate prior authorization requests.
Initial focus areas include:
- Skin and tissue substitutes
- Electrical nerve stimulators
- Knee arthroscopy for osteoarthritis
By identifying high-risk services early, this process helps reduce waste before the service is rendered.
Clinician Oversight
While AI supports the review process, only licensed clinicians are authorized to issue approvals or denials. AI tools cannot make final decisions, ensuring that human clinical judgment remains central to patient care.
17 Services Subject to Prior Authorization (2026 – 2031)
Between January 1, 2026, and December 31, 2031, the following services will be subject to prior authorization in participating states:
- Electrical nerve stimulators
- Sacral nerve stimulation for urinary incontinence
- Phrenic nerve stimulators
- Deep brain stimulation (essential tremor, Parkinson’s)
- Vagus nerve stimulation
- Induced lesions of nerve tracts
- Epidural steroid injections (excluding facet joint injections)
- Percutaneous vertebral augmentation (PVA)
- Cervical spinal fusion
- Arthroscopic knee lavage and debridement
- Hypoglossal nerve stimulation (obstructive sleep apnea)
- Incontinence control devices
- Diagnosis and treatment of impotence
- Percutaneous image-guided lumbar decompression
- Bioengineered skin substitutes for chronic lower extremity wounds
- Cellular/tissue-based wound care products (CTPs) for lower extremities
No Change to Medicare Coverage or Payment
The WISeR Model is designed to enhance Medicare oversight without disrupting patient care or provider reimbursements. Specifically, it:
- Does not change Medicare coverage or payment policies
- Does not affect Medicare Advantage plans
- Only applies to Original Medicare
- Maintains full patient access to covered services and providers
- Excludes services where review delays could compromise patient safety
What This Means for Providers and Patients
For Providers:
Eligible providers in pilot states can choose how to engage with the model. Those with strong compliance histories may receive exemptions, reducing future administrative tasks and streamlining claims processing.
For Patients:
Beneficiaries will continue to receive the same services covered under Original Medicare. There will be no change to coverage, no change in providers, and no added steps for patients.
References
- WISeR (Wasteful and Inappropriate Service Reduction) Model
https://www.cms.gov/priorities/innovation/innovation-models/wiser
- CMS Launches New Model to Target Wasteful, Inappropriate Services in Original Medicare
https://www.cms.gov/newsroom/press-releases/cms-launches-new-model-target-wasteful-inappropriate-services-original-medicare

